Laparoscopic Cruroplasty and Fundoplication
Repair of Hiatal Hernia
Hiatal Hernia:
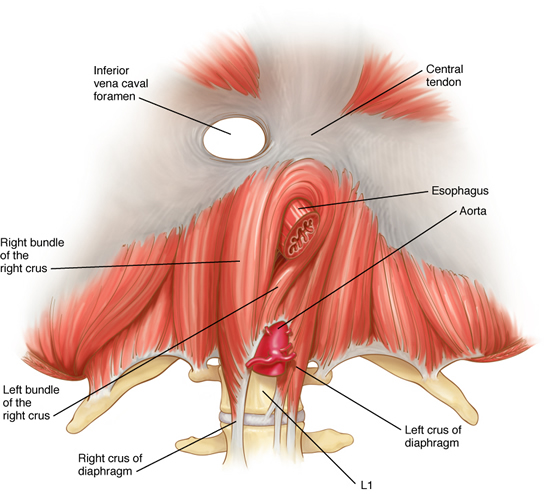
The esophagus passes through an opening in the diaphragm (i.e. esophageal hiatus) as it courses through the chest to the abdomen eventually ending at the stomach. This opening is usually adequate for passage of the esophagus and nothing else. However, patients that have a hiatal hernia have an enlarged opening. There are four different types of hiatal hernias described. The sliding hernia is the most common of the four representing more than eighty-percent of all hiatal hernias. The lower esophageal sphincter- the high pressure zone near the junction of the stomach and esophagus- fails and allows stomach contents to reflux into the esophagus.
Symptoms:
- The symptoms associated with hiatal hernia are variable but generally include:
- Heartburn – 30 – 60 minutes after eating
- Regurgitation – worsened with lying flat
- Excessive belching
- Aspiration – stomach contents refluxed into the airway
- Asthma – chronic result of aspiration
- Chest pain – burning mid-chest pain
- Difficulty swallowing
- Pain with swallowing
- Bleeding
- Stomach twisting and perforation
- Obstruction
Diagnosis:
Several studies are helpful to your doctor in making the diagnosis of hiatal hernia including:
- Chest X-ray:
- Air fluid level in the chest
- Esophagram:
- Assess the function of the esophagus
- Identify structural abnormalities (twisting of the stomach)
- Reveal associated problems (e.g. aspiration, poor gastric emptying)
- Upper endoscopy:
- Identify damage caused by reflux (e.g. Esophagitis, Barrett’s esophagus, malignancy)
- Biopsy esophagus for evaluation of malignancy
- Esophageal manometry:
- Assess the function of the LES
- Assess the wave-like motion (propulsive function) of the esophagus
Surgery:
Laparoscopic Cruroplasty and Nissen fundoplication is the procedure of choice for repair of a hiatal hernia. Patients that have paraesophageal hernia which allows the fundus to be displaced into the chest above the GE junction or patients with other abdominal organs (e.g. spleen, colon, liver) displaced into the chest should be repaired urgently. Repair will help prevent complications such as bleeding, intestinal disruption, strangulation and the like. Elective repair is recommended only for patients that are asymptomatic and have a sliding hernia. This group of asymptomatic patients may also be followed clinically seeking surgery only when symptoms arise.
In the past, open surgery was the only option for repair. This approach is associated with prolonged recovery time and a large painful incision. With the new minimally invasive approach, surgery is now a viable initial therapy even for patients who are asymptomatic.
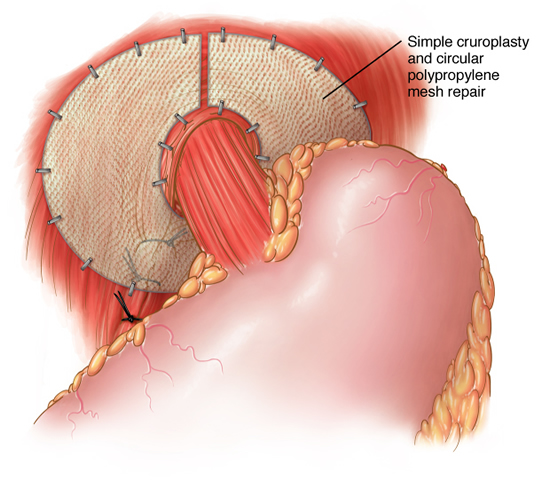
The laparoscopic cruroplasty and Nissen fundoplication is performed through five quarter-inch incisions through which, a camera and instruments are placed. The hernia is reduced from the chest into the abdomen. This may require separation of abdominal organs from the lung and middle chest structures. The hiatus is then re-approximated to the appropriate size. Some hernias are so large and tissues are so poor that prosthetic material must be used to prevent recurrence. After adequate repair of the hiatus, a new lower esophageal valve is constructed by wrapping a two-centimeter portion of the stomach around the lower most portion of the esophagus. This collar is then anchored to the tough fibers of the diaphragm. The procedure typically lasts for two to four hours depending on the size and contents of the hernia. Patients are started on clear liquids the next morning and are discharged in the afternoon. The open surgical technique involves an 8-10 inch upper abdominal incision with a hospital stay of 5-7 days.
Dr. Frantzides initiated and completed a 10 year prospective randomized study in which he included patients who underwent laparoscopic hiatal hernia repair with and without mesh. He found that instead of a 20-35% recurrence rate the use of mesh would reduce or eliminate recurrences. This study was published in 2002 in the Archives of Surgery.
Recovery:
Patients recover sooner after laparoscopic cruroplasty and Nissen fundoplication. Return to activities can occur within 2-7 days compared to 4-6 weeks with an open approach. Wound infections occur less frequently with the laparoscopic technique. Also, less pain has been reported with laparoscopy. Most importantly, greater than ninety-percent of patients are symptom free ten years after the procedure.
Pertinent References
Hiatal Hernia ; Frantzides CT, Carlson M. (on the web/epocrates) https://online.epocrates.com/u/2963735/Hiatal+hernia
Frantzides, C.T., Madan AK,Carlson MA, Zeni TM, Zografakis JG, Moore RE, Meiselman M, Luu M, Ayiomamitis G; Laparoscopic Revision of Failed Fundoplication and Hiatal Herniorrhaphy. J. Laparosc. Adv. Surg. Tech. 19(2): 133-139, 2009
Frantzides, CT, Carlson M; Laparoscopic Hiatal Herniorrhaphy; In Atlas of Minimally Invasive Surgery Frantzides, Carlson (ed.) Elsevier 2008.
Frantzides, C.T., Madan AK, Zografakis JG, Smith C: Laparoscopic Repair of Incarcerated Diaphragmatic Hernia. J Laparoendosc. Adv. Surg. Tech. 17: 39-42, 2007.
Carlson MA, Frantzides, C.T. Laparoscopic Repair of Paraesophageal Hiatal Hernia. Surg. Endosc. 18(12):1821, 2005
Madan AK, Frantzides, C.T., Patsavas KL; “The Myth of the Short Esophagus;” Surgical Endoscopy 18(1): 31-34, 2004
Carlson MA, Frantzides, C.T.: Mesh-Reinforced Repair of Diaphragmatic Hernia (In: V. Schumpelick, L.M. Nyhus (eds) Springer: Meshes: Benefits and Risks pp. 28-289, 2003
Frantzides, C.T., Madan AK, O’Leary PJ, Losurdo J. Laparoscopic Repair of a Recurrent ChronicTraumatic Diaphragmatic Hernia; American Surgeon 69(2):160-162, 2003
Frantzides C.T., Madan AK, Carlson MA: A prospective, randomized trial of polytetrafluoroethylene (PTFE) patch repair vs. simple cruroplasty for large hiatal hernia. Arch. Surg, 137:649-652,2002
Frantzides C.T., Carlson MA: Paraesophageal Herniation in: Baker, RJ and Fischer JE (Eds), Mastery of Surgery, Little Brown Fourth Edition, 2001.
Frantzides C.T, Carlson MA: Laparoscopic Repair of a Congenital Diaphragmatic Hernia in an Adult: A Case Report. Laparoscopic Adv. Surg. Tech., 10:287-90, 2000.
Frantzides CT, Carlson, MA, and Richards CG: Laparoscopic repair of large hiatal hernia with Polytetrafluoroethylene. Surg Endosc. 13:906-908, 1999.
Frantzides CT, Carlson MA: Prosthetic reinforcement of posterior cruroplasty during laparoscopic hiatal herniorrhaphy. Surg Endosc 11: 769-771, 1997